Matrix-induced AutologousChondrocyte Implantation (MACI)
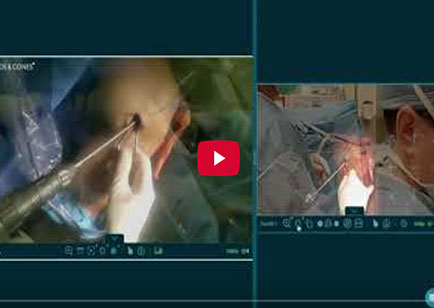
Dr. Garcia’s Live Demonstration of TTO combined with MACI procedure
Check out Dr. Garcia’s demonstration of a MACI biopsy and MACI of the trochlea
-
Video testimonial after MACI patella, MPFL reconstruction and TTO.
-
Check out our recent video testimonial after the MACI procedure for a cartilage defect of the knee.
MACI for Cartilage Repair
MACI (Matrix-induced autologous chondrocyte implantation):
Visit the company website for further details and other videos: www.maci.com/patients/how-maci-works/the-maci-procedure.html
Introduction
Articular cartilage injuries of the knee are common and can significantly affect an individual’s quality of life. These injuries can result from trauma, repetitive stress, or degenerative conditions, leading to pain, swelling, and impaired function. Articular cartilage has a limited ability to heal due to its avascular nature, making effective treatment challenging. One promising treatment option for cartilage repair is Matrix-induced Autologous Chondrocyte Implantation (MACI). This website will review the background of cartilage injuries, the MACI procedure, indications for its use, surgical techniques, outcomes, and rehabilitation protocols.
Recent testimonial after MPFL/TTO/MACI patella in a young athlete
Background of Cartilage Injury
Cartilage Structure and Function
Articular cartilage is a smooth, white tissue that covers the ends of bones where they come together to form joints. It provides a low-friction surface for joint movement and acts as a cushion to absorb shock. The cartilage matrix consists of water, collagen fibers, proteoglycans, and chondrocytes. Chondrocytes are the only cells found in healthy cartilage and are responsible for maintaining the extracellular matrix.
Mechanisms of Injury
Cartilage injuries can occur due to:
- Trauma: Direct blows or falls can cause focal damage to the cartilage.
- Repetitive Stress: Activities such as running or jumping can lead to microtrauma and degeneration over time.
- Degenerative Conditions: Osteoarthritis involves the progressive breakdown of cartilage.
Challenges in Cartilage Repair
The avascular nature of cartilage means it lacks a blood supply, which is crucial for the healing process. Without blood flow, the natural healing response is limited, often resulting in incomplete repair or continued degeneration.
Dr. Garcia demonstrates his cartilage defect treatment using MACI
Background for MACI
What is MACI?
Matrix-induced Autologous Chondrocyte Implantation (MACI) is an advanced technique for repairing cartilage defects. It involves harvesting a patient’s own chondrocytes, culturing them, and then implanting them onto a scaffold that is placed into the defect site. This approach aims to promote the regeneration of hyaline-like cartilage.
History and Development
MACI evolved from the earlier technique of Autologous Chondrocyte Implantation (ACI), which was first introduced in the 1990s. ACI involved injecting cultured chondrocytes directly into the defect, but it had limitations such as cell leakage and difficulty in securing the cells. MACI improves on this by using a collagen membrane to hold the cells in place.
Advantages of MACI
- Better Cell Retention: The scaffold ensures that the chondrocytes stay within the defect site.
- Improved Integration: The membrane provides a framework for new tissue formation.
- Minimally Invasive: The surgical procedure can be performed arthroscopically, reducing recovery time.
Dr. Garcia’s MACI of the patella, TTO, MPFL reconstruction in high definition
Indications for MACI
Patient Selection
MACI is indicated for patients with:
- Focal Cartilage Defects: Localized damage rather than widespread degeneration.
- Symptomatic Lesions: Pain, swelling, and mechanical symptoms that impair function.
- Failed Conservative Treatment: Non-surgical measures such as physical therapy and medication have not provided relief.
Contraindications
MACI is not suitable for:
- Diffuse Osteoarthritis: Generalized cartilage loss throughout the joint.
- Joint Instability: Conditions like ligament injuries that need to be addressed first.
- Infection or Inflammatory Diseases: Active infections or inflammatory conditions such as rheumatoid arthritis.
Surgical Process and Technique
Preoperative Planning
- Diagnostic Imaging: MRI and X-rays to assess the extent of the defect.
- Arthroscopy: Direct visualization of the joint to confirm the lesion’s size and location.
The MACI Procedure
The MACI procedure is performed in two stages: cartilage cell harvesting and implantation.
Stage 1: Cartilage Cell Harvesting
During the first stage, the surgeon performs an arthroscopic procedure to collect a small sample of healthy cartilage from a non-weight-bearing area of the knee. This sample is sent to a specialized laboratory where the chondrocytes (cartilage cells) are isolated and expanded over a few weeks.
Stage 2: Cartilage Implantation
Once the chondrocytes have multiplied, they are embedded onto a collagen membrane, creating the MACI implant. In a subsequent surgery, the damaged cartilage is debrided (cleaned) to create a suitable bed for the implant. The MACI implant is then precisely placed over the defect and secured with fibrin glue or sutures.
Full MACI, TTO, MPFL with Rods and Cones Video Technology
Surgical Procedure
- Cartilage Biopsy: A small sample of healthy cartilage is taken arthroscopically.
- Cell Culturing: The harvested chondrocytes are sent to a lab where they are cultured for 4-6 weeks to increase their numbers.
- Second Surgery: The cultured cells are seeded onto a collagen scaffold.
- Implantation: The scaffold is trimmed to fit the defect and secured in place using fibrin glue or sutures.
What happens during the second surgery?
Generally, these MACI implantations need to be done open, though future advances may offer arthroscopic method for certain defect. If the patella is involved frequently a tibial tubercle osteotomy is needed as well. For a trochlear defect we can sometimes do these in isolation. We use the MRI to determine if a tibial tubercle osteotomy is needed and calculate the amount of correction needed to protect the MACI implant. We may also add other surgical procedures to improve the patient’s outcome (ie MPFL reconstruction or high tibial osteotomy).
Depending on the combined second procedures the patients will be non-weightbearing for 2-6 weeks. Usually, a continuous passive motion machine is needed for 2-3 weeks after surgery to ensure your knee is bending smoothly to improve growth of the MACI. Please review Dr. Garcia’s rehab protocols for specifics on each surgical recovery.
Postoperative Care
- Wound Care: Keeping the surgical site clean and dry.
- Pain Management: Medication to control pain and swelling.
- Protected Weight Bearing: Use of crutches or braces to protect the repair site.
Outcomes
Clinical Outcomes
- Pain Relief: Many patients experience significant pain reduction.
- Improved Function: Increased ability to perform daily activities and sports.
- Long-term Durability: Studies show that MACI can provide durable repair for several years.
MACI of the Patella
Complications
- Infection: Risk of postoperative infection, though rare.
- Graft Failure: Failure of the implanted cells to integrate and form new cartilage.
- Overgrowth of Repair Tissue: Hypertrophy of the new cartilage, which may require additional surgery.
Outcomes and Benefits of MACI
MACI has shown promising outcomes in terms of pain relief, improved knee function, and enhanced quality of life. Studies have reported high patient satisfaction and durable results over long-term follow-up. Advantages of MACI over other cartilage repair procedures include
- Use of Autologous Cells: Since the patient’s own cells are used, there is no risk of rejection or disease transmission.
- Natural Cartilage Regeneration: The procedure promotes the growth of hyaline-like cartilage, which is more like native cartilage compared to fibrocartilage formed in other procedures.
- Longer Term Studies: The MACI procedure has one of the most robust track records with numerous research studies demonstrating good results with long term follow up.
What are the outcomes after surgery?
Overall, the results are quite good after surgery. Success rates are upwards of 80-85% success for a most scenarios. Return to sports rates are also high as well. Success rates drop to 65-70% if both the patella and trochlea are involved ie “kissing lesions” so it is important to take care of these cartilage defects before the wear becomes that extensive.
Rehabilitation Protocol
Phase 1: Immediate Postoperative (0-6 Weeks)
- Immobilization: Brace to protect the knee and limit movement.
- Cryotherapy: Ice packs to reduce swelling.
- Range of Motion Exercises: Gentle exercises to maintain joint flexibility without stressing the repair site.
Phase 2: Early Rehabilitation (6-12 Weeks)
- Weight Bearing: Gradual increase in weight-bearing activities.
- Strengthening Exercises: Focus on quadriceps and hamstring strengthening.
- Low-impact Activities: Swimming or cycling to improve cardiovascular fitness without stressing the knee.
Phase 3: Progressive Rehabilitation (3-6 Months)
- Advanced Strengthening: Increasing resistance and intensity of exercises.
- Proprioceptive Training: Balance and coordination exercises.
- Functional Drills: Sport-specific drills to prepare for return to activity.
Phase 4: Return to Activity (6-12 Months)
- Gradual Return to Sports: Based on individual progress and physician recommendations.
- Maintenance Program: Ongoing exercises to maintain strength and flexibility.
- Regular Follow-ups: Monitoring by the healthcare team to assess progress and address any issues.
Complications:
- Overgrowth of the implant ie (the MACI cartilage grows too much)
- Infection
- Bleeding
- Stiffness
- Lack of MACI growth
Overall complications are low, and Dr. Garcia will review these during the pre-surgical discussion
Conclusion
Matrix-induced Autologous Chondrocyte Implantation (MACI) offers a promising solution for patients with focal cartilage defects in the knee. By utilizing the patient’s own cells and a supportive scaffold, MACI aims to regenerate hyaline-like cartilage, providing long-term pain relief and improved joint function. While the procedure requires careful patient selection, meticulous surgical technique, and a comprehensive rehabilitation protocol, the outcomes can be highly rewarding for those who undergo this treatment. With ongoing advancements in cartilage repair technologies, MACI represents a significant step forward in the management of cartilage injuries.
For more information visit the MACI website at: www.maci.com/patients/how-maci-works/the-maci-procedure.html
-
Testimonial after MACI with MPFL Reconstruction
-
Check out our recent MACI case presentation for a trochlea defect in a young athletic patient
-
My recent MACI talk with Dr. Brian Cole on how to maximize cartilage training in fellowship.
-
Testimonial after 3 Part MACI and TTO
-
3 Part MACI with TTO testimonial
-
MACI overgrowth and treatment
-
MACI Trochlea 2025 Testimonial
-
Staged ACL Repair with MACI, TTO and MPFL reconstruction
-
MACI, TTO, MPFL 2025 Testimonial