Proximal Tibiofibular Instability and Stabilization
Proximal tib-fib stabilization using the cutting edge tightrope technique
Proximal Tibia and Fibula Instability and Stabilization: Insights from an Orthopedic Surgeon
As an orthopedic surgeon with extensive experience, I encounter patients presenting with proximal tibia and fibula instability. This condition, often overlooked in general discussions about knee injuries, can significantly impair functionality and quality of life. In this detailed overview, I aim to shed light on the anatomy, common injuries, symptoms, diagnostic approaches, nonoperative treatments, and indications for surgical intervention.
Anatomy of the Proximal Tibia and Fibula
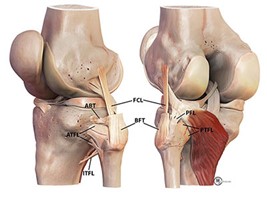
The proximal tibia and fibula are key components of the knee joint and lower leg. The tibia, or shinbone, is a major weight-bearing bone, crucial for standing and walking. The fibula, though smaller and non-weight-bearing, provides important muscle attachments and stabilizes the lateral aspect of the knee and ankle. The proximal tibiofibular joint is a relatively small joint where the tibia and fibula meet near the knee. This joint, along with the ligaments surrounding it, including the anterior and posterior tibiofibular ligaments, plays a vital role in knee stability and function.
Injuries Leading to Instability
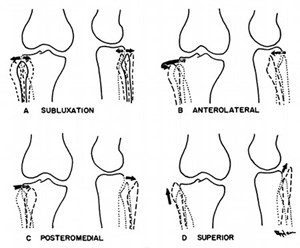
Instability at the proximal tibiofibular joint typically results from direct trauma or rotational injuries. These can include:
- High-energy impacts: Such as in sports or vehicular accidents.
- Twisting injuries: Often occurring in activities involving rapid changes in direction.
- Falls: Particularly those that involve twisting the knee while the foot is planted.
Symptoms and Examination
Patients with proximal tibia-fibula instability often report:
- Lateral knee pain: Especially noticeable during activities that stress the joint.
- Swelling: Around the lateral aspect of the knee.
- Instability or “giving way” sensations: Particularly during rotational movements.
During an examination, I focus on:
- Palpation: Checking for tenderness over the proximal tibiofibular joint.
- Assessment of joint stability: Using specific maneuvers to test the integrity of the joint and its ligaments.
- Range of motion: To identify any restrictions or pain during movement.
**Imaging, including X-rays and MRI, can be instrumental in confirming the diagnosis and ruling out other knee pathologies. Often imaging does not confirm the diagnosis. This is generally a diagnosis of physical examination and history.
Nonoperative Treatment
The initial approach to managing proximal tibia and fibula instability often involves conservative measures:
- Rest and Ice: Critical for reducing inflammation and pain.
- Compression and Elevation: Aids in managing swelling.
- Physical Therapy: Focuses on strengthening the muscles around the knee, improving joint stability, and restoring the range of motion.
- Bracing or Taping: Can provide additional support and stability to the joint during the healing process. Taping can be useful for providing proprioceptive feedback during rehabilitation. This is always done before considering any surgical fixation. This is a excellent diagnostic test, and can I add significant treatment value as well.
When to Consider Surgery
Surgical intervention may be considered in cases where:
- Conservative treatments fail: Continuing symptoms of instability or pain despite appropriate conservative management.
- Significant ligamentous injury: As demonstrated by imaging
- High-demand athletes or active individuals: Where joint stability is paramount for performance.
Surgical Options
When nonoperative treatments are not effective, surgery may be necessary to restore stability and function. Surgical options vary based on the severity and specifics of each case.
- 1. Arthrodesis: Arthrodesis, or joint fusion, is typically reserved for severe cases. The procedure involves fusing the tibia and fibula together, eliminating motion at the syndesmosis joint to provide stability. This surgery has fallen out of fever and is not recommended any further.
- 2. Reconstruction: Ligament reconstruction involves replacing the damaged ligaments with grafts to restore stability. This can be an autograft (from the patient) or an allograft (donor tissue). This has been the gold standard for several years but newer techniques, as mentioned below, are starting to gain more traction for this rare surgical condition.
- 3. Tight Rope Fixation: A newer technique, tight rope fixation, involves placing a strong suture between the tibia and fibula, which maintains the space and stability of the syndesmosis joint. This method allows for more physiological movement compared to traditional screw fixation. There are numerous case reports, and this has become the most cutting-edge treatment for these patients. It does not burn any bridges in the future, and if reconstruction is needed after tight rope fixation this does make the surgery any more difficult.
Dr. Garcia is one of the few surgeons in Washington state that perform this surgery and has experience in reconstruction as well as the newer tightrope fixation and will offer each surgery option is a customize approach based off the patient’s history, imaging and physical examination.
Extensive Detail on Surgical Options
Arthrodesis
- Procedure: Removal of cartilage from the joint, followed by the placement of screws or plates to hold the bones together.
- Recovery: It includes a period of non-weight bearing, followed by gradual introduction of weight-bearing activities.
Reconstruction
- Procedure: Harvesting of graft, followed by drilling holes in the tibia and fibula to place the graft, replicating the original ligaments.
- Recovery: Involves immobilization in a cast or boot, followed by physical therapy.
Tight Rope Fixation
- Procedure: Placement of a high-strength suture through small drill holes in the tibia and fibula. The suture is then tensioned to stabilize the syndesmosis.
- Recovery: Typically involves less immobilization time than traditional methods and a quicker return to activities.
Surgical Outcomes
Surgical intervention for tibia-fibular instability generally has positive outcomes. Patients often experience:
- Improved stability and function in the ankle.
- Reduced pain and discomfort.
- Enhanced ability to perform daily activities and return to sports.
Physical Therapy and Rehabilitation
Post-surgical rehabilitation is crucial for optimal recovery. It typically involves:
- Initial Phase: Focus on reducing swelling and pain while protecting the repair through controlled exercises.
- Middle Phase: Gradual introduction of weight-bearing exercises and strengthening routines.
- Final Phase: Advanced exercises focusing on balance, agility, and returning to normal activities.
Contact Dr. Garcia’s office for evaluation. If you think you or a friend is suffering from this condition, we are happy to evaluate and recommend appropriate non-operative or operative treatment.