Fertilized ACL Reconstruction
Fertilized ACL Technique
Biologically Augmented Anterior Cruciate Ligament Surgery for Enhanced Healing and Recovery
Podcast Update on the Bio ACL
Background
Anterior cruciate ligament (ACL) injuries are among the most common and significant knee injuries, especially in athletes and active individuals. Standard ACL reconstruction has evolved over the years with improvements in graft selection, surgical technique, and rehabilitation protocols. However, one of the major limitations of conventional ACL surgery is the reliance solely on mechanical reconstruction without addressing the biologic environment of the healing graft.
Fertilized ACL reconstruction is a novel, biologically enhanced approach that aims to accelerate graft healing, improve integration into the bone tunnels, and optimize long-term outcomes. The term “fertilized” refers to augmenting the surgical construct with biologic agents-such as bone marrow aspirate concentrate (BMAC), demineralized bone matrix (DBM), and platelet-rich plasma (PRP)-to create an enriched environment for graft incorporation.
This technique represents the next frontier in sports medicine, blending traditional surgical reconstruction with cutting-edge biologic science.
Indications
Fertilized ACL reconstruction can be considered in any patient undergoing ACL reconstruction, particularly those who meet one or more of the following criteria:
- High-performance athletes seeking the best chance at a safe and rapid return to sport.
- Revision ACL reconstruction where biologic healing potential may be compromised.
- Younger patients (<25 years old) who are at higher risk for re-rupture.
- Patients with tunnel widening or poor bone quality who may benefit from biologic enhancement.
- Patients undergoing concurrent procedures such as meniscus repair or cartilage surgery.
It is also commonly used in patients who have sustained an ACL tear and express interest in the most advanced surgical techniques available to promote biologic healing.
Important Note on Coverage:
The biologic components used in fertilized ACL reconstruction - BMAC, DBM, and PRP - are not typically covered by insurance and represent an additional out-of-pocket cost. However, many patients consider the investment worthwhile given the potential benefits in graft healing and recovery.
Imaging
A thorough imaging workup is essential for planning an ACL reconstruction, whether traditional or biologically enhanced.
MRI:
- Confirms the ACL tear and assesses for associated injuries (meniscal tears, bone bruising, cartilage damage).
- Evaluates graft remnants, tunnel position (in revisions), and joint effusion.
X-rays:
- AP, lateral, and tunnel views are used to assess bony anatomy and any prior hardware.
- Standing alignment views may be helpful in certain patients, especially those with chronic instability.
Optional:
- CT scan may be indicated for revision cases with tunnel malposition or widening.
Imaging plays a key role in identifying patients who may particularly benefit from biologic augmentation, such as those with tunnel widening or concurrent cartilage loss.
Surgical Options
Traditional ACL Reconstruction:
- The torn ligament is removed and replaced with a graft (autograft or allograft).
- Bone tunnels are drilled in the femur and tibia, and the graft is fixed with screws or suspensory fixation devices.
- Healing depends on the incorporation of the graft into the bone tunnels and revascularization over time.
Fertilized ACL Reconstruction:
This technique uses the same mechanical reconstruction approach as traditional surgery but adds biologic components to enhance healing:
- BMAC (bone marrow aspirate concentrate): Harvested from the iliac crest or tibial metaphysis, containing stem cells and growth factors.
- PRP (platelet-rich plasma): Derived from the patient’s own blood, rich in platelets and cytokines that promote tissue regeneration.
- DBM (demineralized bone matrix): Serves as a scaffold to enhance bone integration in the tunnels.
Together, these biologics are placed into the femoral and tibial tunnels and around the graft to create a biologically active environment that may improve graft incorporation and healing.
Surgical Technique
Fertilized ACL reconstruction follows the general principles of anatomic ACL reconstruction but with the added biologic augmentation steps.
Step-by-Step Overview:
- Graft Harvest:
- Typically a bone-patellar tendon-bone (BTB) autograft or hamstring autograft.
- Allograft may be used in selected patients.
- Tunnel Preparation:
- Anatomic femoral and tibial tunnels are drilled under arthroscopic guidance.
- Tunnel size and orientation are optimized for graft placement.
- Biologic Preparation:
- Bone marrow is aspirated and concentrated using a centrifuge.
- PRP is isolated from a venous blood draw.
- DBM is mixed with BMAC and PRP to form a biologic “graft extender.”
- Graft Placement:
- The ACL graft is passed through the tibial and femoral tunnels.
- Before final fixation, the biologic mixture is injected into the tunnels around the graft.
- Fixation:
- The graft is secured using standard interference screws or cortical fixation.
- Additional PRP may be injected intra-articularly at the end of the procedure.
- Closure and Dressing:
- Standard wound closure.
- A sterile dressing is applied, often with a cryotherapy or compression system postoperatively.
The biologic components act to “fertilize” the healing zone, potentially accelerating incorporation of the graft and reducing tunnel widening, one of the common issues seen in standard ACL reconstruction.
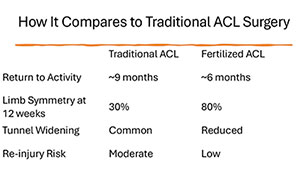
Differences in Outcomes Compared to Standard ACL Reconstruction
While traditional ACL reconstruction is highly successful in most patients, there are some areas where biologic augmentation may offer advantages:
| Outcome Measure | Standard ACL | Fertilized ACL |
|---|---|---|
| Graft incorporation time | 12–16 weeks | Potentially shortened to 8–12 weeks |
| Tunnel widening | Occurs in up to 30% | Reduced in biologically treated tunnels |
| Return to sport timeline | 9–12 months | May be accelerated in some cases |
| Revision rate (high-risk patients) | Up to 10–15% | Early studies show potential reduction |
| Meniscal healing when repaired | Variable | Improved biologic environment may help |
Several ongoing studies, including prospective clinical trials, are evaluating long-term outcomes of fertilized ACL reconstructions. Early data suggests improved early graft healing and potential reductions in tunnel expansion and re-injury rates.
Complications
The complication profile for fertilized ACL reconstruction is similar to traditional ACL surgery, with some additional considerations:
Standard Surgical Risks:
- Infection
- Graft rupture or failure
- Tunnel malposition
- Stiffness or arthrofibrosis
- Deep vein thrombosis (DVT)
Biologic-Specific Considerations:
- Donor site morbidity (e.g., iliac crest soreness from BMAC aspiration)
- Increased surgical time due to biologic preparation
- Cost: The biologic components (BMAC, DBM, PRP) are not usually covered by insurance and must be paid for out-of-pocket.
- Uncertain long-term benefit: While promising, biologics are still under investigation and long-term superiority over standard methods is not definitively proven.
Recovery
Recovery after fertilized ACL reconstruction is similar in structure to standard ACL rehab but may offer advantages in graft incorporation and biologic healing.
Postoperative Timeline:
- Day 0–2 Weeks:
- Weight bearing as tolerated with crutches.
- Range of motion (ROM) exercises initiated immediately.
- Emphasis on quad activation and edema control.
- Weeks 2–6:
- Progressive strengthening and ROM.
- Stationary bike, pool therapy.
- Weeks 6–12:
- Advance to closed-chain strengthening.
- Light jogging and balance training.
- Months 3–6:
- Sport-specific drills and agility training.
- Months 6–9:
- Return to high-level sports, pending strength, neuromuscular control, and functional testing.
Patients undergoing fertilized ACL reconstruction often meet return-to-play milestones slightly earlier, though clearance still depends on objective functional recovery, not just time alone.
Outcomes
Preliminary outcomes of fertilized ACL reconstruction are encouraging:
- Improved MRI signal intensity of graft at 3–6 months post-op, suggesting faster incorporation.
- Reduced tunnel widening observed on follow-up imaging.
- Faster quadriceps strength recovery in some cohorts.
- Higher patient satisfaction scores, especially in revision or high-demand populations.
While long-term comparative studies are still maturing, the biologically augmented approach holds significant promise, especially in high-risk populations where graft healing is paramount.
Conclusion
Fertilized ACL reconstruction is an exciting advancement in orthopedic sports medicine that aims to enhance graft healing through biologic supplementation. By combining traditional surgical principles with regenerative techniques such as BMAC, PRP, and DBM, this procedure offers the potential for faster recovery, stronger graft integration, and reduced failure rates-particularly in younger, athletic, or revision cases.
Patients should be aware that while the mechanical aspects of the surgery are standard, the biologic components are not typically covered by insurance and may incur an additional cost. A detailed discussion with your orthopedic surgeon will help determine if this advanced procedure is right for you.
If you’re considering ACL reconstruction and are interested in maximizing healing potential and long-term success, biologically fertilized ACL reconstruction may be a valuable option.